The following story is dedicated to Amanda Lavelle, a close family friend who recently had a severe case of meningitis; multiple doctors neglected to diagnose her infection, resulting in an extensive recovery process and surgery to fix the acute problem. Do not ignore symptoms in yourself or in your family and friends, seek medical help; if you have a feeling, keep pushing for tests and confirmed diagnosis!
Original publication
1965 marked the invention of Kevlar, a protective high strength fabric. Centuries before Kevlar, through elegant biological structures, the human body developed a tough and protective membrane of its own, made for the brain and spinal cord — the meninges.
When infected, the meninges —the last line of defense for the central nervous system — swell, pressuring the brain and spinal cord to fatal levels. We call this inflammation meningitis.
On Feb. 11, junior economics major Nicolis Williams died of bacterial meningitis. Currently, the Brazos County Health Department is investigating his case to find others potentially at risk.
“Really, our investigation focuses on close contacts with the individual. We’re looking at trying to protect the population that has been exposed,” said Kate Jackson, an epidemiologist for the health department.
Those who lived near Williams and were in contact with him present higher risks of developing meningitis; the incubation period for bacterial meningitis spans a full week.
“It’s very rare that we find someone like that; they’re not going to get tested unless they’re really sick,” Jackson said. “It could even be someone who was vaccinated and got a very light case of it and then passed it on.”
While the investigation continues, appearance of another case is not likely.
“We worry about outbreaks, but the majority of cases in the United States are sporadic, few and far between,” said Dr. Tom Clark, a medical epidemiologist for the Center for Disease Control and Prevention. “It is transmitted from person to person, but really requires relatively close contact.”
Health professionals oftentimes describe meningitis as similar to the flu.
“That’s part of the problem with the diagnosis, that it’s most often the flu, and it’s only sometimes more serious,” Clark said. “Part of it, too, is that the signs and symptoms, especially of bloodstream infections, are fairly subtle.”
“[A defining symptom of meningitis] is usually a pretty sudden onset of fever,” Clark said.
Over 10 to 12 hours, symptoms might develop to full potency, even causing death within a day. With treatment, meningitis may be handled with confidence and relative ease, though early diagnosis remains a necessity. A particularly sudden onset of fever, headache or an aching neck, especially all together, calls for an immediate visit to a clinic or emergency room.
“If there’s any suggestion of symptoms or signs of meningitis, then you should certainly [have] a spinal tap. It’s a pretty routine procedure, but you can’t always do it at the time,” Clark said. “Meningitis is actually in some ways better because it is kind of a localized infection, and the bacteria themselves are more susceptible to the antibiotic treatments.”
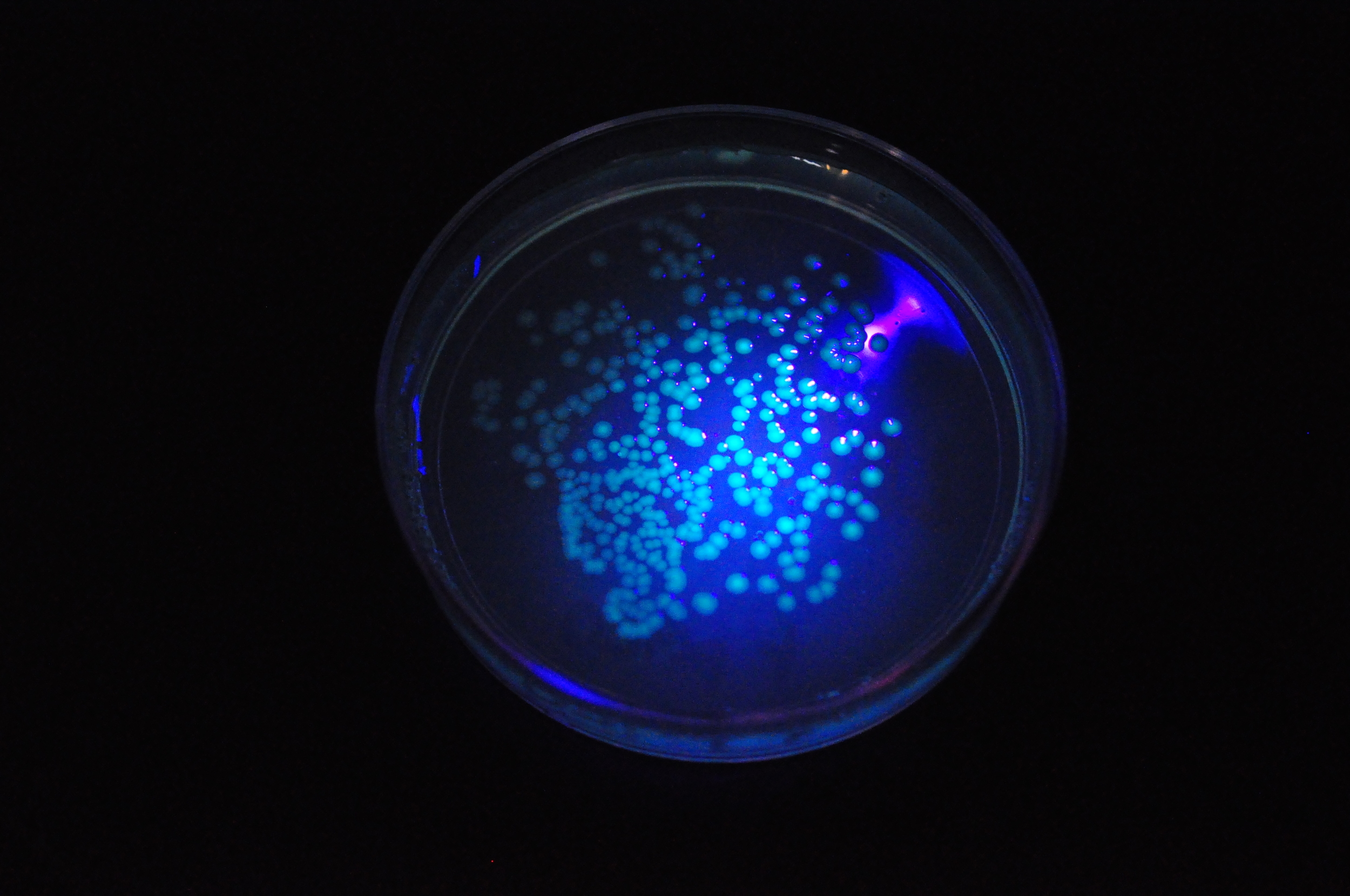
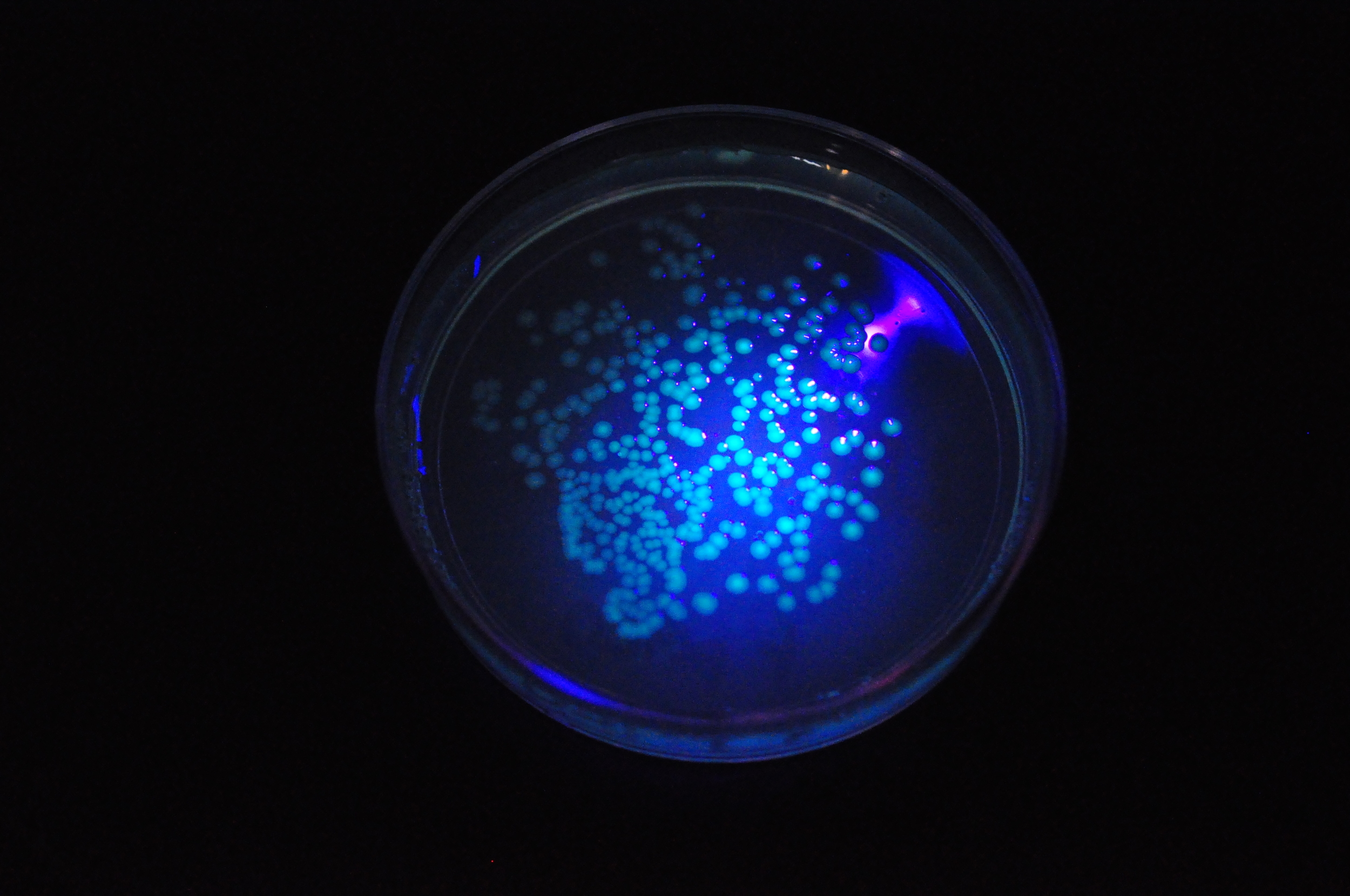
Though basic tests may indicate meningitis and support treatment, the only way to be certain is through a culture of the infecting agent — a test that requires a spinal tap. A spinal tap may be inconceivable due to the progression of the infection or due to injuries and other physical obstacles, but meningitis may still be determined with other indicators.
“Usually the doctor can do some quick maneuvers in the office to determine if you have meningitis,” said Dr. John Simmons. Simmons is an assistant professor in the Texas A&M Health Science Center for the College of Medicine.
A spinal tap requires only an hour for preliminary suggestion for antibiotic regimen, though 48 hours is required for a complete test result.
“A lumbar puncture, or a spinal tap, sounds like this awful thing, but it’s really a common side procedure that takes only 10 to 15 minutes,” Simmons said. “Anytime you stick someone with a needle there is risk for a minor injury, but the risk of any serious injury from a lumbar puncture is exceedingly rare.”
Simmons said the spinal tap procedures are most commonly associated with childbirths. However, Simmons said people should not hesitate to seek medical treatment because they fear the procedure.
Other tests include attempting to touch one’s chin to chest; a bending of the knees during the maneuver indicates inflexibility due to swelling and pain. Also, doctors may have a patient recline and raise their legs; if the patient cannot manage to extend their legs while raised, it may indicate a similar swelling in the spine.
“The risk of meningitis is about one in 100,000. That risk is increased in freshmen dorms because you have so many people living in close proximity,” Simmons said. “Most people are no longer immune because it has been more than five years since they received their vaccination.”
In the case of Nicolis Williams, a vaccine was not required for his off-campus living arrangements. Unconfirmed reports stated that a few days prior to admittance to College Station Medical Center, Williams visited A.P. Beutel Health Center with flu-like symptoms.
“We’re primarily ambulatory, acute care,” associate director of the center Scott Draper said, “We don’t have surgical or overnight capabilities. We’re actually very fortunate to have EMS here, staffed 24/7. We feel very fortunate that we have that resource here for our students and our campus,” Draper said. “And the student fee helps to support that service and those resources being on campus.”
Medicine constantly changes, research and technology achieve breakthroughs in efficiency and diagnostic power, and even in treatment; the student health center employees said they work hard to keep with the curve.
“About three years ago we went out and bought digital radiography equipment because that is the new standard of care,” Draper said, “We’re constantly looking at how we can improve patient care and access.”
Renovations are an ongoing process in the center to keep up, currently with the addition of examination space in their first-floor pods.
“We’re striving to be the benchmark in college health; we’re not perfect, but we’re trying to be,” Draper said.